Is there a link between poor digestive function and depression?
If you’ve been diagnosed with depression, your doctor may have told you that you’re ‘just born that way’, and you may worry that having a depressed family member means that you’ll get depression too. However, science is showing that our destinies are not written in our genes and that depression is often a symptom of chronic inflammation.
Inflammation can be defined as a localized reaction that produces redness, warmth, swelling, and pain as a result of infection, irritation, or injury. And the western diet (high in salt, sugar and low in fresh fruits, vegetables, whole grains and legumes) causes inflammation and can lead to and exacerbate symptoms of depression.
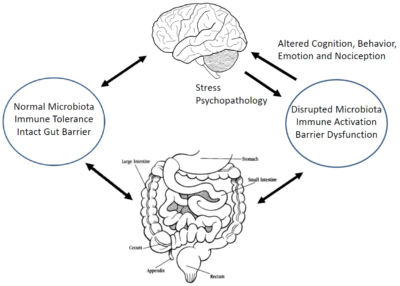
Think of your gut as your ‘second brain’. It’s easy to see the link between the two – butterflies when you’re feeling excited, no appetite when you’re stressed or worried. The enteric nervous system (ENS) is the cellular lining that covers our entire gastrointestinal tract, from your oesophagus to your rectum; it sends signals to the brain via millions of nerve cells. This ‘second brain’ is revolutionising medicines understanding of the links between digestion, mood, health and even our thought processes.
Researchers are finding evidence that irritation in the gastrointestinal system sends signals to the central nervous system that triggers mood changes. This may explain why a higher than normal percentage of people with functional bowel problems develop depression and anxiety. Controversially, it’s been shown that some gastroenterologists prescribe certain antidepressant medications for patients with IBS, illustrating the link between the two.
The western diet and lifestyle is creating an epidemic of poor digestion with gas, bloating, pain and exhaustion after meals. Diagnosis of gastrointestinal disorders like Crohn’s, Colitis, and Irritable bowel are rising worldwide. Always listen to your gut: if you come back after lunch feeling exhausted, nauseous or foggy your ENS may be reacting to something you ate and sending signals to your brain.
Here at Core, we work with food sensitivity tests to enable us to obtain a more individualised picture and use diet as a tool to help with reducing inflammation in order to gain effective results.
Learn more about food sensitivities and how they differ from food allergies here and feel free to ring us with your questions.